Controlling your asthma
Asthma management devices can help deliver your or your child's medication more effectively while reducing side effects1, 2.
Understanding how asthma management can help
Why is it so important to manage your asthma? Asthma management devices can help deliver your or your child’s medication more effectively, while reducing side effects1,2. By getting the right level of medication to your lungs, at the right frequency your healthcare professional has prescribed, you can live life with fewer symptoms and more freedom.
Many people living with asthma think their condition is managed well if symptoms flare up only occasionally, and assume that using an inhaler less means their asthma is more in control. In fact, that can mean your asthma treatment plan isn’t working as well as it should or that you aren’t adhering to it as prescribed. But side effects from taking medication—like the taste or the feel of it in the back of your throat—can discourage you from sticking to your plan.
Take control! See how our asthma management devices can help manage your asthma.
The aim of treatment is to manage your asthma so that7:
Are you in control of your asthma?
Take the quick test to find out
The Global Initiative for Asthma (GINA) recommends using questions such as the following to assess asthma control7:
1. If you or your child has asthma, do you or your child have coughing, wheezing, or chest tightness more than twice a week? Yes or No
2. If you or your child has asthma, does it limit you or your child from participating in sports or normal physical activities? Yes or No
3. If you or your child has asthma, do you or your child wake up at night with asthma symptoms? Yes or No
4. If you or your child has asthma, do you or your child use your rescue inhaler more than twice a week to treat asthma symptoms? Yes or No
If you answered yes to any of these questions, your or your child’s asthma may not be well controlled and you should schedule an appointment with your healthcare professional to discuss symptoms and review your asthma action plan.
Indoor Air quality matters
Take control of the indoor air
With 24,000 breaths taken every day, the air in our homes can impact our lives. Better air quality can help prevent or alleviate allergies, asthma and respiratory issues, so we can all breathe a little easier. Philips Air solutions reduce four major factors that influence indoor air quality: Allergens – such as pollen coming in from outdoors, dust mites, pet dander (flakes of skin) and mold spores. Air humidity or dry air – this can aggravate allergies, asthma and other respiratory conditions.
Air in our homes is often 2–5 times more polluted than outdoor air. Everyday activities — like cooking, cleaning and playing with pets — all release allergens and air pollutants into the home.
PM 2.5 – the microscopic air pollutants that are common triggers for an asthma attack.
Air Purifiers:

Philips Air purifiers remove 99.97%1 of airborne allergens including pollen, house dust mites and pet dander2.
Certified by authorities such as AHAM, ECARF.
Thanks to exclusive AeraSense technology, a particle sensor that detects even a slight change in the air and ensures the purifier’s settings are adjusted to reduce airborne allergens.
1 Particles between 0.3 and 10 microns 2 Tested on the filter media for 1 pass efficiency at 5.33cm/s air flow, by a third party lab.
Air Humidifiers:

Philips Air humidifiers retain comfortable moisture levels in your home by maintaining a constant and even, relative humidity between 40% and 60%.
Philips Air humidifiers spread 99% less bacteria compared to ultrasonic humidifiers3 thanks to exclusive NanoCloud Technology.
They distribute the humidified air in the room evenly.
3 Compared to standard ultrasonic technology (non warm mist), Philips NanoCloud technology emits up to 99% less natural bacteria into the air, as tested for 8 weeks in a 1m3 chamber, and certified in an independent laboratory benchmark study by Rabe HygieneConsult in June 2012 (Rabe Hygiene Consult 2101p_12.116).
2-in-1 Air Dehumidifier & Purifier:

Philips 2-in-1 Air dehumidifier and purifier reduces moisture and allergens for a drier, healthier home.
Philips 2-in-1 Air dehumidifier and purifier filters ultra-fine particles as small as 0.02 microns4 thanks to NanoProtect filter.
Get real-time feedback from the air quality indicator and digital humidity display.
4 The filter was tested with NaCl test aerosol according to DIN71460-1 in IUTA
In order to get more tips on how to manage your child's asthma at home and school, see below:
Aiming for the green zone on your asthma action plan
An asthma action plan is a document that you can create together with your healthcare professional that outlines when and how much asthma controller medication you or your child should take daily to manage your condition, how often to use reliever medication and what additional steps to take if symptoms get worse.
A simple green-yellow-red format makes it easy to track whether you are doing well or getting worse, and what to do about it. Used along with a peak flow meter to track your lung function, the action plan can help you stick with your treatment for better overall asthma management.
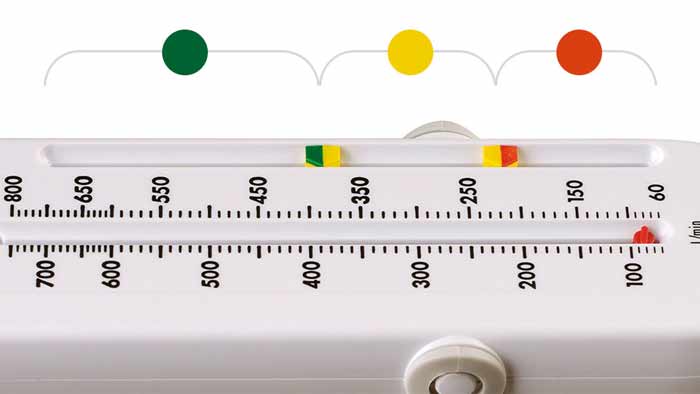
The three zone traffic light system with Philips PersonalBest peak flow meter
Improve medication delivery

Medicine often ends up in your mouth, throat and stomach when using an inhaler on its own. A valved holding chamber (sometimes called a spacer) may improve drug delivery to the lungs where it is needed by as much as up to 4 times4. Getting the right amount of medication can help reduce day-to-day symptoms and keep you in the green zone2.
Track your peak flow for better control of your asthma

A peak flow meter is used to measure how fast you blow out air from your lungs.
A peak flow meter is also used to determine if your asthma symptoms are putting you into the yellow or red zone of your asthma action plan.
Get medication to your lungs where it is needed

Your healthcare professional may prescribe reliever medication delivered by a pMDI inhaler or nebulizer for breathing treatment of worsening asthma symptoms. Nebulizers turn liquid medication into a fine mist that is more easily absorbed into your lungs. The goal is to get your or your child back to the green zone and doing well.
InnoSpire Go
Portable mesh nebulizer

Fast, effective and easy to use, the InnoSpire Go portable mesh nebulizer is designed to shorten asthma treatment time by 25%5, so your medication can be delivered in as little as four minutes.6 Virtually silent, InnoSpire Go is small, portable, discreet and can be used anywhere.
See InnoSpire Go and learn how it works

Get the facts
Read more about common myths about asthma

Ask your healthcare professional or pharmacist about asthma management
Your healthcare professional or pharmacist can be valuable resources for understanding the use and benefit of including asthma management devices as part of an asthma action plan. Some asthma management devices are available only with prescription.
Breathe easier at home
Helping you manage the indoor air quality you and your family are exposed to, keeping your home clean and healthy.
Frequently asked questions
DISCLAIMER:
Information on this website is informational only and should not replace the advice of a physician.
FOOTNOTES: [2] Asthma.org.uk. Advice/inhalersmedicines.treatments/inhalers-and-spacers. Accessed January 2016. [3] Asthma.org.uk. Advice/manage-your-asthma. Accessed January 2016. [4] Gardenhire D., Arzu A., Dean H., Myers T. A guide to aerosol delivery devices for respiratory therapists 3rd edition, American Association for Respiratory Care, 2013. [5] Versus predecessor, Aeroneb Go. [6] Using 2.5ml salbutamol.
[1] Newman, S.P., et al. Improvement of pressurized aerosol deposition with Nebuhaler spacer device. Thorax, 1984; 39(12) 935-41
[7] ginasthma.org. 2017-gina-report-global-strategy-for-asthma-management-and-prevention. Assessment of Asthma page 29. Accessed November 2017.
You are about to visit a Philips global content page
Continue









